Systems-level thinking is key to success in ablation device product development
Companies developing new surgical energy (ablation) therapies usually treat each “component” separately. One team of mostly electrical and software engineers develops capital hardware, a different team specialized in mechanical engineering of high-volume disposables develops an instrument or catheter, and yet another team (usually with little product development knowledge at all) specifies and tests the performance in tissue or animal models.
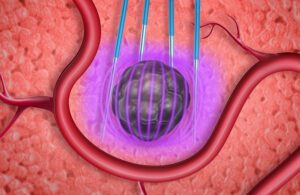
In pulsed field ablation, electronic fields kill cells through irreversible electroporation. [Illustration courtesy of Minnetronix]
While effective for resource management, this approach leaves no one responsible for understanding and intentionally designing for the interactions between capital, instruments, and tissue, a set of interactions that is often a late-stage surprise when system integration occurs and the therapy doesn’t work as expected.
A more robust approach begins with an appreciation of these interactions and plans to ensure they are a deliberate part of the design. To illustrate the impact of this problem, here are three common examples where a lack of systems-level approach trips up the inexperienced design team.
Cabling
Something as benign as positioning of wires within a cable assembly can radically change its performance, especially when cables are carrying high frequencies such as those in radiofrequency (RF) ablation or high-current pulses in pulsed field ablation.
A mechanical engineer designing a cable is likely to produce an arrangement that is optimal from a mechanical perspective (flex, twist, manufacturability) but inferior for performance in a surgical energy system due to parasitic coupling between wires, leakage currents, and other non-idealities. Knowing what cable and instrument design parameters are important from an electrical perspective can result in major performance improvements with only minor changes to the cable design.

Figure 1) Poor cable layup (left) results in undesirable capacitive coupling compared to an arrangement with greater inter-wire spacing (right). [Illustration courtesy of Minnetronix]
Figure 1 illustrates two cable cross-sections that appear superficially similar, yet one configuration dramatically reduces undesirable inter-wire capacitive coupling, improving the system’s ability to accurately measure important parameters such as tissue impedance. The impact of this difference is often not appreciated until the “wrong” design is built, a problem is found, and a lengthy and frustrating investigation finally pinpoints the error — and no one is happy to find that the only solution is to scrap miles of custom cable and redesign an expensive extrusion die.
Temperature measurement
Many surgical energy systems rely on accurate temperature measurement to deliver effective therapy, yet fail to appreciate the system-level sources of inaccuracies and imprecision.
Thermocouples are a popular temperature measurement device for their low cost and small size, yet it may not be understood that thermocouples are only relative temperature measurement devices. They rely on an absolute temperature measurement device elsewhere in the system, and their best-case accuracy is only realized when the sum of these individual sensor inaccuracies is minimized.

Figure 2) A catheter handle with misplaced absolute temperature sensor becomes inaccurate when held in user’s warm hand. [Illustration courtesy of Minnetronix]
Figure 2 shows a situation where failure to understand this principle manifested in a surgical energy device that relies on temperature measurement for efficacy and safety, but rapidly loses accuracy when held in the user’s warm hand.
Control systems
A vehicle’s cruise control may report being set to 60 mph, but the first encounter with a hill makes it obvious that slight variation around this setpoint is part of normal operation. The same is true in any medical device that relies on a control system to maintain a set temperature, impedance, flux, power, or other parameter.
In fact, the best performance of such a closed-loop system depends on minimizing errors in three different variables:
Total Error = [error in power source] + [error in sensor(s)] + [control error]
While designers may expend great effort in minimizing errors, they often fail to appreciate that control error is an unavoidable artifact of any closed-loop system and thus must be planned for in a formal error budget.
Additionally, much like how a vehicle’s cruise control behaves differently on a flat road versus on a hill, control system errors have both steady-state and transient behaviors. Understanding the transient response is often critically important, yet rarely receives sufficient attention.
Avoid pitfalls by adopting best practices
The start of any new surgical energy product design should begin with the appointment of a technical leader responsible for ensuring that disparate teams are aware of, and planning for, the most salient system-level interactions.
While technical leadership in medical device development is often delegated to a systems engineer, experience in writing and testing requirements is not necessarily concomitant with the multi-disciplinary technical breadth needed to offer great technical foresight.
Selecting the right technical leader is as important to your product development’s success as any executive hiring decision you may make, much as finding an experienced design team is key to a meeting your schedule and budget.

Daniel Friedrichs [Photo courtesy of Minnetronix]
Daniel Friedrichs, PhD, is a surgical energy technical expert who leads development engineering efforts at Minnetronix Medical, a design, development and manufacturing partner to leading medical device companies around the world. He is named on more than 35 patents and has worked with an extensive network of clients seeking to commercialize a wide array of technologies.
Source:MDO









