How the Shockwave Reducer implant is designed to treat refractory angina
It’s been three years since the FDA denied approval to the Neovasc Reducer system for treating refractory angina.
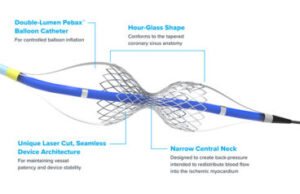
The investigational Shockwave Reducer implant is designed for patients with refractory angina. [Image courtesy of Shockwave]
At the time, the device developer already had a CE mark on the catheter-delivered coronary implant and breakthrough device designation from the FDA, but struggled to explain exactly how it worked. That was one of the shortcomings identified in October 2020 by the Circulatory System Devices Panel of the Medical Devices Advisory Committee to the FDA when nearly all of those experts said they were not convinced of the system’s effectiveness.
Now Shockwave Medical owns the technology through its 2023 acquisition of Neovasc. The intravascular lithotripsy (IVL) system developer — itself purchased by Johnson & Johnson for $13.1 billion this year — is conducting clinical trials to support Reducer’s next shot at FDA review in the U.S., aiming for FDA approval sometime around 2027.
Shockwave sees a $5 billion market for Reducer, estimating that 500,000 patients in the U.S. in Europe have refractory angina with no obstructive coronary arteries (ANOCA). The company believes the prevalence of refractory angina will increase due to “progressively longer life expectancy of patients.”
The Shockwave Reducer procedure
Shockwave Medical is best known for its IVL systems that fracture arterial calcium before implantation of a vessel-expanding stent for blood flow restoration.
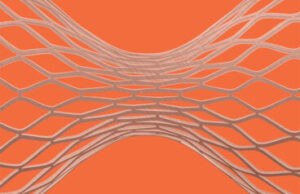
The investigational Shockwave Reducer implant is made of laser-cut stainless steel and delivered via a minimally invasive catheter procedure. [Image courtesy of Shockwave]
While the investigational Reducer system is also designed for revascularization, Shockwave says it does this by narrowing the heart’s largest vein, the coronary sinus, where deoxygenated blood drains into the right atrium.
The Reducer implant is an hourglass-shaped, bare metal device made of laser-cut stainless steel. This balloon-expandable implant is placed in the heart’s coronary sinus with a minimally invasive catheter procedure.
It starts with an ultrasound-guided catheter puncture in a patient’s jugular vein, first with a 6-Fr multipurpose angiographic (MPA) catheter sheath and then a 9-Fr delivery sheath, according to Dr. Hakim Benamer, a paid Shockwave consultant who discussed Reducer at Euro PCR, the annual meeting of the European Association of Percutaneous Cardiovascular Interventions (EAPCI).
This “mother-child” catheter technique allows for pressure monitoring with the MPA catheter sheath inside the delivery sheath. A contrast injection confirms positioning and appropriate oversizing of 10-20% compared to the diameter of the coronary sinus before the balloon expands the Reducer device.
“The perfect landing zone is when you have a valve just after the angulation and before the distal branch of the sinus,” said Benamer, an interventional cardiologist at Hôpital Privé Jacques Cartier in France.
Shockwave says the implantation procedure requires minimal training and takes about 20 minutes once the 0.035-in. guidewire has accessed the coronary sinus. (Watch a video from Shockwave showing the procedure at the end of this post.)
How the Reducer limits flow to relieve angina symptoms
Understanding the mechanism of action of a drug or device can help physicians decide whether and how to use it to treat a patient. But it’s not always clear how drugs or devices work, said Dr. James Spratt, consultant cardiologist at St George’s University NHS Trust in London..
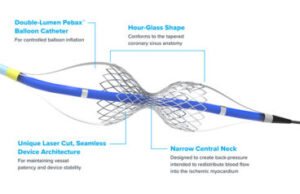
This illustration from Shockwave Medical shows the design features of the Reducer implant. [Image courtesy of Shockwave]
“Metformin is … probably the most prescribed drug in the world, which we know works really well for lots of things, but we still don’t really know how it does it,” Spratt said. “It’s not always clear how things work even though they have clear benefit.”
Spratt, who like Benamer is also a paid consultant to Shockwave, explained the Reducer’s proposed mechanism of action in another 2024 presentation at Euro PCR.
The Reducer implant’s hourglass shape was designed to conform to the tapered anatomy of the coronary sinus, allowing for placement as long as the narrowest part of the vein is less than 13 mm in diameter.
The device’s narrow central neck throttles the flow of blood through the coronary sinus, creating back-pressure. Shockwave says that pressure redistributes blood into a patient’s ischemic myocardium (heart muscle), relieving the symptoms of refractory angina.
“We put in the Reducer [and] we increase the resistance to the venous draining. and like with any flow system that pressure is translated back to the venous system,” Spratt said. “… That reinflates the venous system and we get this kind of pressure transmission across the arterial side and we get reinflation of these compressed arterials.”
“This is the hard bit to get your head around, how the increase in venous pressure could lead to a reduction in resistance to arterial flow,” he continued. “I think probably the closest medical equivalent is CPAP where you have compressed lungs, you put pressure into the lungs and you reinflate the lungs, therefore you get reduced resistance of flow.”
The back-pressure from the Reducer implant is designed to improve perfusion of the endocardium, helping to relieve ischemia and chest pain, shortness of breath and other debilitating symptoms, Shockwave says.
While Spratt said he himself is still improving his understanding of the complex physiology at play, the procedure itself doesn’t have much of a learning curve.
“I think you’re comfortable [after placing] five implants,” he said. “Having a background in complex PCI (percutaneous coronary intervention) is pretty helpful because we see those patients in need and we also — I hope — understand the difference between futility and feasabilty and also the risk that some of these patients are [taking]. In my practice I would probably consider the Reducer in patients I wouldn’t have done five or 10 years ago, particularly post-bypass patients with diffuse disease.”
“I also think we all need to take a step back and be a bit more realistic about what revascularization does achieve [and] the limits of revascularization,” he continued. “Physiology’s got a lot to teach us about what revascularization can achieve. Some humility in the field would be probably overdue.”
Article Source: Medical Design









