Catheters: How to Achieve Optimal Hypotube Design

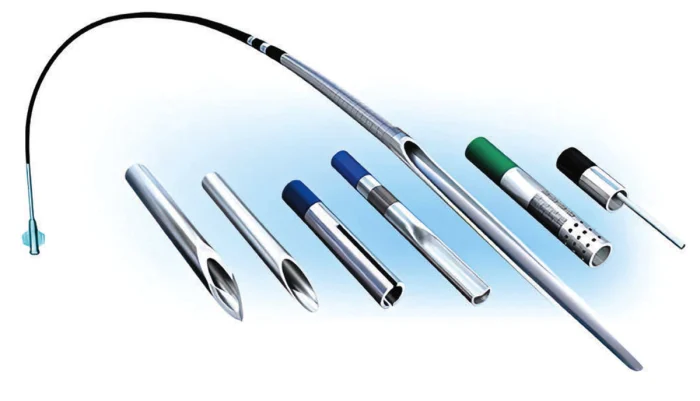
In minimally invasive surgery, the best patient outcome begins with navigating the vasculature safely and smoothly. For catheters utilizing a metal shaft construction, good design begins with a high-performing hypotube. This article provides insights and guidance on hypotube development and manufacturing for successful product design. It also presents the key manufacturing processes required to create the ideal access or delivery catheter.
THE ROLE OF THE HYPOTUBE
A hypotube provides essential performance characteristics to enable access and delivery within the vasculature including flexibility, push, torque, track, kink resistance, lubricity, and fast inflation and deflation times. However, these characteristics can present tradeoffs; for example, a hypotube optimized for maximum flexibility can exhibit low push forces. When designing a hypotube, it is essential to understand these performance characteristics and how optimization of one characteristic can impact others to achieve the perfect balance for the product.

In minimally invasive surgery, the best patient outcome begins with navigating the vasculature safely and smoothly. (Credit: Freudenberg Medical)
This section explains the key performance characteristics of the hypotube and how these characteristics translate to the physician experience when deploying a catheter within the patient.
Torque. The anatomical pathways of the vasculature can be challenging to navigate, often tortuous or highly calcified. It is essential that the physician can rotate the minimally invasive device within the vasculature to reach the target treatment site and torque, a twisting force, aids device rotation. The ability of a device to accurately transmit this torque along its length is measured as torque-ability. When torque forces are not accurately transmitted, it can lead to a buildup of force and an undesirable whipping effect along the device shaft. Innovative processing techniques can ensure that hypotube shafts will deliver the necessary amount of torque, with predictability of movement when rotating.
Pushability. Pushability is determined by the measure of the transmission of longitudinal forces from the proximal to the distal end of the catheter. Ideally, when a pushing force is applied by the physician, an equal movement of force should be exhibited on the distal tip inside the patient. When transmission forces are high, the physician navigates with confidence, knowing that precise movements to the proximal shaft will translate to precise movements within delicate anatomical pathways or structures, for example, within the crucial anastomotic circle of Willis structure during neurovascular navigation.
When designing a hypotube, optimization of one characteristic can impact others to achieve the perfect balance for the product. (Credit: Freudenberg Medical)
Trackability. The term trackability is used to measure the overall ability of a device to progress through complex vasculatures and reach the treatment site. Sometimes, a physician will refer to trackability as the overall feel of the device or how smoothly it responds to the physician’s manipulation. When low tracking forces are present, the physician feels that the device is easier to manipulate and position. The distal, or treatment end of the catheter, plays a crucial role in overall trackability. Advanced processing technologies can make the distal end of the catheter more flexible, thus aiding trackability.
Flexibility. Flexibility is a measure of the stiffness along the hypotube length and is a critical part of the overall catheter design. Flexibility is a major contributor to the trackability or feel of the device and, while high pushability or stiffness is desirable, a well-designed hypotube should simultaneously exhibit good flexibility when it is required to navigate acute angles or anatomical structures. Optimizing flexibility and pushability together is key to the perfect hypotube design.
Lubricity. Lubricity measures how much the friction between the medical device and the anatomy or companion device is reduced through the application of a coating to the metal hypotube. Freudenberg Medical, for example, offers a differentiated coating solution called Cambus Coat™, which has proven to exhibit excellent adhesion and resistance to flaking under the most demanding performance tests. Additionally, Cambus Coat™ is a smooth lubricious coating solution ideal for hypotube and guidewire applications.
Kink Resistance. Intravascular anatomy is challenging to navigate and requires the physician, on occasion, to cross acute radii. Kink resistance measures the hypotube’s ability to maintain an intact cross functional profile when bent around a radius. This characteristic is critical in preserving the patency of the internal lumen which plays a critical role in therapy delivery. With this criticality in mind, an advanced metallurgical solution with superior kink resistance over traditional 304 stainless steel hypotube constructions such as Freudenberg Medical’s E-Pro™ should be considered. In addition, such a solution offers product designers an opportunity to optimize internal diameters.
Inflation and Deflation Time. In addition to being a critical tool in vascular navigation, the hypotube plays an essential role in delivering balloon catheter therapies. Inflation and deflation times describe the length of time it takes an angioplasty balloon to activate and deactivate. When inflated, a balloon creates a temporary restriction of blood flow, which can be damaging to downstream anatomy unless it is precisely and accurately controlled. The inner diameter of the hypotube plays a crucial role in determining the balloon inflation and deflation time. In short, the larger the internal diameter of the hypotube, the faster balloon inflation and deflation response.

A hypotube provides essential performance characteristics to enable access and delivery within the vasculature. Its characteristics translate to the physician experience when deploying a catheter within the patient.
MANUFACTURING THE OPTIMAL HYPOTUBE
An extensive range of capabilities are required to manufacture the optimal hypotube, balancing the performance characteristics discussed above. This section reviews the key technical capabilities required to deliver a tailor-made minimally invasive catheter.
Electrical Discharge Machining (EDM). EDM is a high-precision machining process used for cutting precision contours in metal material. This method produces burr-free skives in thin-wall tubing. A well-designed skive enables a smooth transition zone between the metal shaft and the distal balloon assembly, improving overall trackability and flexibility of the catheter.
Laser Cutting. Hypotubes must navigate complex and tortuous paths, therefore requiring specific bend radii and flexibility. Laser cutting provides various cut geometries assisting with flexibility, torque and compression. Advanced laser cutting profiles can be used for steerable, high-load catheter applications.
Passivation. Hypotube manufacturing employs a range of processing techniques to add or remove features from the metal tube. These processes can introduce contaminants (free iron) on surfaces, and it is essential that all contaminants are removed from the hypotube. Freudenberg Medical, for example, passivates all of its stainless steel hypotubes to the international passivation standard ASTM A 967. Passivation and electropolishing chemically dissolve contaminants on the stainless steel surface, forming a thin protective chromium oxide layer on the steel, which gives it’s a stainless quality.
Laser Ablation. Marker bands on a coated hypotube surface help a physician estimate the longitudinal placement of the catheter relative to key anatomical structures as it is introduced into the vasculature. Automated laser systems remove PTFE coating from the outer diameter of the hypotube to create these markers at various intervals along the shaft.
Centerless Grinding. Centerless grinding is a machining process that uses abrasive cutting to remove material from a metal shaft. A highly accurate outer diameter, thinner walls, or intricate features on the hypotube outer profile can be achieved through this grinding process.
Laser Welding. State-of-the-art laser welding systems can produce spot-welded and seam-welded joints in producing corewire and other micro-welded assemblies. This welding capability enables engineers to manufacture a hypotube shaft with advanced form, shape, or profile features for the addition of transition elements such as distal core wires.
PTFE Coating. PTFE coating is a popular finish on a hypotube’s outer diameter, providing high lubricity to improve device trackability. Cambus Coat™, a PFOA-free coating, for example, offers the highest levels of adhesion over traditional methods.
Pad Printing. An alternative method to create the femoral, brachial, and radial marker bands discussed above is through the application of a contrasting-colored ring around the outer coated surface of the hypotube using a process called pad printing. The PTFE hypotube surface is typically black in color and the pad-printed marker band is typically white to optimize contrast and visibility in the cath lab.
Inspection. Product quality and consistency are paramount in medical device manufacturing. Material testing and inspection must be an integral part of manufacturing processes and should always follow documented procedures and systems that comply with customer’s requirements.









