Critical Issues in Remote Monitoring: Data Capture and Quality
Before the pandemic, forward-thinking care providers and health systems were trialing virtual care solutions that could bridge the facility to the home, seeking connected care models that work for their systems and patients. Yet, before 2020—connected health to the home or in the house was at the periphery of healthcare.
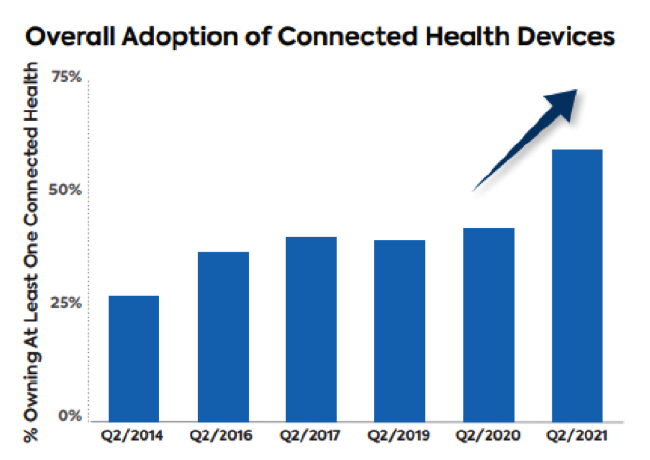
Figure courtesy of Parks Associates
Today, many virtual care solutions have a weakness: They are remote visits only and lack the means to gather important vital signs and clinical testing data. This significantly confines telehealth use cases—limiting the use of virtual solutions in tracking chronic conditions, in monitoring patients at an elevated risk of complications due to a disease state, those who are pre-or post-surgery, and others who may benefit from tracking data. While remote patient monitoring programs integrate data capture and monitoring capabilities, many suffer from user experience flaws, resulting in low compliance rates.
In August 2021, the Mayo Clinic released a study of more than 7,000 patients across 41 states who had participated in RPM programs for COVID-19 treatment. The study found the remote treatment to be safe and effective, but even this well-designed program from a national leader does not achieve full compliance. Overall, 79% of respondents engaged with the RPM technology, meaning they engaged and received at least one day of monitoring. Additionally, on average, patients complied with 60–70% of the self-reporting of vital signs or symptoms tasks scheduled or assigned. Yet, that still means that participants failed to self-report 30–40% of required vital signs or symptoms.
Several critical issues can potentially impact the effectiveness of remote care programs in the home such as device pairing, user reporting errors, user discomfort, intermittent data, and lack of overnight monitoring.
As more healthcare activities occur from home, continuous monitoring solutions—including those that can track a patient’s status overnight—and new technology like artificial intelligence will be critical to support communications between providers and patients. Solutions that offer continuous and passive monitoring will play a crucial role in helping to fill the gaps, particularly in assessing patient deterioration or important changes in health conditions.
The development of smart sensors and the decreasing costs of devices have made it possible to offer chronic disease management, aging-in-place and post-acute care services in the home. Truly continuous patient monitoring at home typically occurs in one of two approaches: Wireless wearable monitoring sensors, patches, and devices or via environmental sensors. Companies taking the first approach use patches and wearable holsters to monitor cardiac and other vital sign information continuously.
Environmental sensors can detect health status passively and are an alternative or complementary source of continuous monitoring, used in healthcare and in the active aging market. Some systems use a combination of smart home sensors and peripheral devices to track users’ activities of daily living and identify anomalies that may indicate abnormal, unhealthy, or emergencies. These exception-based alerts may involve unexpected activities (entries and exits, bathroom visits, kitchen visits) or wellness notifications (prolonged inactivity, higher or lower than expected activity).
As sensors can capture new data throughout the day, they can establish individuals’ typical routines and normal activities. For instance, if someone does not open the refrigerator door in the morning, an alert could be set to help alert someone of this unusual/out-of-the-norm activity.
Models of remote healthcare in the home are both scaling and evolving. Innovative players in this space are rolling out well-designed and user-intuitive health IoT solutions, pulling in data from sensors and devices in consumers’ homes, and building intelligent, integrated platforms that better serve their clients and patient populations. Changes in reimbursements have also helped accelerate the adoption of new approaches to monitoring that, instead of sending data straight to medical records and putting the burden of viewing and interpreting data on clinicians, call on intelligent platforms to analyze the data and escalate to clinicians if appropriate.
There remains a need for solutions that can remove the burden of compliance from the end-user and give providers insights into patient health status in-between readings and overnight. With continuous, connected passive sensors and devices supporting healthcare models in the home, there’s a new opportunity to elevate the experience for both the provider and the patient. The future of healthcare requires non-invasive solutions that enable providers to understand and manage healthcare events for consumers proactively. Sensor-based technologies that provide passive monitoring will continue to play a huge role in healthcare in the future.
Article source: Medical Design Briefs









