Mending broken hearts
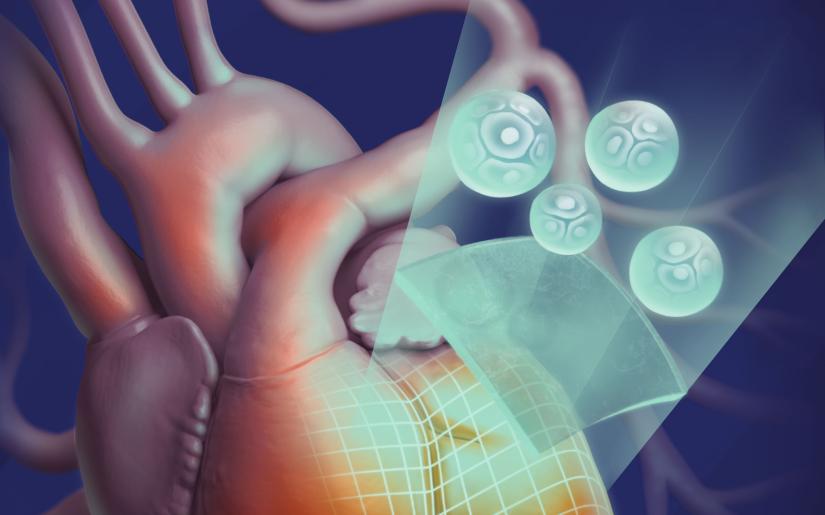
A new technology that uses bio-printed ‘patches’ to repair damaged heart tissue has been proven to be safer and more cost-effective for patients.
Researchers from The University of Technology Sydney (UTS) have demonstrated that bio-engineered heart tissues can safely and effectively help patients recover from the damage caused by an extensive heart attack.
The findings have been published in the world-leading academic journal, Bioprinting.
The new technology creates personalised ‘bio-inks’ made of a patient’s own stem cells. The ‘bio-inks’ are then used to 3D-print cardiac tissues to repair areas of dead tissue caused by heart attacks.
“Thanks to our study we have a better understanding of how bioengineered heart tissues work in the body after their transplantation,” said Dr Carmine Gentile, head of the Cardiovascular Regeneration Group at UTS.
“Our study demonstrated that bio-engineered patches were the best and most robust treatment of heart failure – patches generated with other approaches either did not induce any improvement or the improvement was inconsistent.
“Our bio-engineered patches promise to be safer, more consistent and cost-effective for the patient.”
Cardiovascular disease is the leading cause of death worldwide. In Australia, it accounts for about one in four deaths – claiming a life every 12 minutes.
Heart failure is a frequent complication of heart disease, with inadequate blood supply resulting in the death of heart tissue in an affected area. Life-long drug therapy may be required as a result, and end-stage heart failure means some patients join the waiting list for a heart transplant.
“Because this technology will enable patients to use their own stem cells to create the heart ‘patches’, not only can they potentially dramatically reduce the trauma and cost of a heart transplant, but also avoid hurdles such as a body rejecting donor tissues,” said Dr Gentile.
Further testing for long term effects of this technology are underway before starting clinical trials.
Heart Research Australia, a key funding partner of the research, commended the advances made by Dr Gentile and his research team in striving to improve the devastating statistics surrounding heart disease.
“It’s wonderful to hear that this research partnership has proven to be successful and is now able to progress to the next stage. We are excited about the potential of this technology to help the hundreds of thousands of people affected by heart failure each year,” said Nicci Dent, CEO Heart Research Australia.
Article Source: UTS









